Progeria 101 / FAQ
What is Progeria?
Hutchinson-Gilford Progeria Syndrome (HGPS or Progeria) is an ultra-rare, fatal, “rapid- aging” disease. Its name is derived from Greek and means “prematurely old.” The classic type is Hutchinson-Gilford Progeria Syndrome, which was named after the doctors who first described it: in 1886 by Dr. Jonathan Hutchinson, and in 1897 by Dr. Hastings Gilford.[1]
How common is Progeria?
Progeria occurs in approximately 1 in 4 – 8 million newborns, affecting both sexes equally and all races. One in 18-20 million living individuals has classic Progeria, and there are an estimated 400 children living with Progeria worldwide. Since The Progeria Research Foundation (PRF) was created in 1999, we have found and helped children with Progeria living in 72 countries and all continents.[2]
What are the features of Progeria?
Although they are usually born looking healthy, most children with Progeria begin to display characteristics of Progeria within the first year of life. Sometimes the earliest signs of Progeria are tightness or bulging of the skin in the abdominal and/or thigh area, and failure to thrive (falling well below the pediatric growth curve). Other early Progeria signs include loss of body fat and hair, skin changes, joint contractures and some telltale x-ray findings. Children reach an average maximum height of 125 cm (49.21 inches) and 25 kg (55.12 pounds). The children have a remarkably similar appearance despite differing ethnic backgrounds. As children get older, they develop accelerated atherosclerosis and cardiovascular (heart) disease. This is the same atherosclerosis that usually affects people in their 60s or older, but it affects those with Progeria much earlier and at a rapid rate.
What is the cause of Progeria?
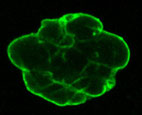
Progeria Cell Nucleus
A group of leading scientists from PRF’s Genetics Consortium including Dr. Francis Collins, then Director of the National Human Genome Research Institute, isolated the Progeria gene. In April 2003, the Consortium reported this finding in the top scientific journal Nature.[3]
“Isolating the Progeria gene is a major achievement for the medical research community,” said Dr. Francis Collins, senior author of the Progeria gene mutation report. “The discovery not only gives hope to children and families affected by Progeria, but also may shed light on the phenomenon of aging and cardiovascular disease.”
The Progeria gene discovery revealed that Progeria is caused by a mutation in the gene called LMNA (pronounced “lamin-A”). The LMNA gene produces the lamin A protein, which is part of the structural scaffolding that holds the nucleus of a cell together and helps to keep cells healthy. The abnormal lamin A protein that causes Progeria is called progerin. Progerin makes cells unstable, which leads to the process of premature aging and disease in Progeria.
What does Progeria have to do with aging?
Perhaps the most exciting clue into the aging process is the discovery that the progerin protein is present at increasing concentrations in both Progeria and normal cells as we age. Our bodies accumulate progerin within the cells of the cardiovascular system at rate of about 3% each year (much lower than in children and young adults with Progeria). Thus, understanding Progeria promises new avenues for understanding the natural aging process.
Children with Progeria are genetically predisposed to premature, progressive heart disease. Death occurs almost exclusively due to widespread heart disease, the leading cause of death worldwide.[4] Thus, there is clearly a tremendous need for research in Progeria. Finding a cure for Progeria will not only help those with Progeria, but may also provide clues for treating millions of adults with heart disease and stroke associated with the natural aging process.
Is Progeria passed down from parent to child?
HGPS is not usually passed down in families. The gene change is almost always a chance occurrence that is extremely rare. Children with other types of “progeroid” syndromes which are not HGPS may have diseases that are passed down in families. However, HGPS is a “sporadic autosomal dominant” mutation – sporadic because it is a new change in that family, and dominant because only one copy of the gene needs to be changed in order to have the syndrome. For parents who have never had a child with Progeria, the chances are one in 4 – 8 million. But for parents who have already had a child with Progeria, the chances of it happening again to those parents is much higher – about 2-3%. Why the increase? This is due to a condition called “mosaicism,” where a parent has the genetic mutation for Progeria in a small proportion of their cells, but does not have Progeria. Prenatal testing during pregnancy is available to look for the LMNA genetic change that causes HGPS in the fetus.
How is Progeria diagnosed?
Because of the historic Progeria gene discovery, we have a definitive, scientific way to diagnose the children. This results in more accurate and earlier diagnoses so they can receive proper care. The Progeria Research Foundation has a Diagnostic Testing Program that looks at the specific genetic change, or mutation, in the Progeria gene that leads to HGPS. After an initial clinical evaluation (looking at the child’s appearance and medical records), a sample of the child’s blood is tested for Progeria. Genetic testing is also available at some genetic diagnostics facilities. Accompanying genetic counseling is always advised.
Is there treatment for Progeria?
Yes! History was made in September 2012, when the results of the first-ever Progeria clinical drug trial demonstrated that lonafarnib, a farnesyltransferase inhibitor (or FTI), was an effective treatment for Progeria[5]. All trial participants experienced significant improvements in weight gain, bone structure, and most importantly, the cardiovascular system.
Two subsequent studies, one from 2018 published in the Journal of the American Medical Association (JAMA)[6], and one from 2023 published in Circulation[7], demonstrated that lonafarnib helped extend survival in children with Progeria.
The 2012 and 2018 studies led to the extraordinary 2020 U.S. Food & Drug Administration (FDA) approval of lonafarnib, now branded as ‘Zokinvy,’ as the first-ever treatment for Progeria. A critical milestone in PRF’s mission, this approval was the culmination of 13 years of clinical research involving four clinical trials, bringing 96 children from 37 countries to Boston for treatment.
With this milestone, Progeria joined the ranks of fewer than 5% of rare diseases with an FDA-approved treatment.
Soon after the FDA approval of lonafarnib, the European Medicines Agency (EMA) approved lonafarnib for use in Europe in July 2022, followed by the Japanese Ministry of Health, Labor and Welfare (MHLW) in January 2024.
Without lonafarnib, the children die of atherosclerosis (heart failure or strokes) at an average age of 14.5 years [6] . With long-term lonafarnib treatment, cardiovascular health is significantly improved, and life expectancy has been shown to increase by an average of 4.5 years7. That’s more than a 30% increase in average lifespan, from 14.5 years to almost 20 years of age!
With the children living longer due to lonafarnib therapy, physicians are seeing aortic stenosis (narrowing of a critical heart valve) as a problem in the older children and young adults with Progeria that may be amenable to lifesaving surgery. In some cases, surgery to insert new heart valves or open blood vessels supplying the heart (stents) has helped to improve the health of patients in later stages of disease[8].
What are the more recent developments in Progeria research?
PRF is heavily involved in the development of three other therapeutic pathways, each of which has shown varying levels of increased lifespan when studied in Progeria mouse models – from 50% to an astonishing 140%! Our goals are to discover new treatments that will work even better than lonafarnib alone, and to eventually cure Progeria by correcting the genetic mutation. We are targeting the disease at the protein, RNA and DNA levels.
- DNA Base Editing: This pathway aims to permanently correct the Progeria gene mutation at the DNA level.
In January 2021, the science journal Nature published breakthrough results demonstrating that genetic editing in a mouse model of Progeria corrected the Progeria mutation in many cells, improved several key disease symptoms and increased lifespan in the mice by 140%[9]. Additional preclinical studies are needed to investigate these results, which we hope will one day lead to a clinical trial.
“To see this dramatic response in our Progeria mouse model is one of the most exciting therapeutic developments I have been part of in 40 years as a physician-scientist,” said Francis Collins, MD, PhD.
- RNA Therapeutics: This pathway aims to stop the production of progerin by correcting the genetic mutation at the RNA level.
In March 2021, PRF contributed to two very exciting breakthrough studies on the use of RNA therapeutics, both of which attempt to block the body’s ability to produce progerin production at the RNA level. One study showed that treating Progeria mice with a drug named SRP2001 reduced the harmful progerin mRNA and protein expression in the aorta, the main artery in the body, as well as in other tissues. At the end of the study, the mice demonstrated an increased survival of 62%[10].
The other study showed a 90 – 95% reduction of the toxic progerin-producing RNA in different tissues after treatment with a drug called LB143. Progerin protein reduction was most effective in the liver, with additional improvements in the heart and aorta.[11]This genetic correction is temporary, thus ongoing treatment to maintain the correction is required. - Small Molecule (Drugs): This pathway aims to reduce the level of the toxic progerin protein that causes Progeria.
A drug called progerinin has shown great promise. In a Progeria mouse model, progerinin increased body weight and extended lifespan by 10 weeks, a substantial breakthrough, compared with lifespan extension of two weeks in lonafarnib-treated mice.[12]The field of Progeria research is making major advancements, continuously growing in scope and sophistication as the search for effective treatments and the cure continues. Brilliant, passionate researchers are leading the field to breakthroughs and new treatments that help children with Progeria live longer, healthier lives, while also driving discovery in heart disease and aging.In addition to exploration of new pathways toward treatments and the cure, in March 2023, PRF reported findings on the discovery of a Progeria biomarker, a new way to measure progerin, the toxic protein that causes Progeria. A biomarker has a game-changing capacity to unlock the promise of smarter and faster drug trials, and better treatments. Using blood plasma to measure progerin levels, researchers can understand how treatments are affecting clinical trial participants after a shorter period of time and at multiple points along each clinical trial, instead of relying on subjective clinical features.This test can optimize the clinical trial process by providing early information about the effectiveness of treatments being tested, as a lead-in to other clinical tests such as weight gain, dermatologic changes, joint contracture and function, etc., all of which require much more time to manifest. We may now be able to understand treatment benefits as early as four months after starting treatment, or stop a treatment that may not benefit the trial participant, to avoid unnecessary side effects.[13]
How is PRF advancing the research toward a future cure, and helping children with Progeria today?
 The Progeria Research Foundation funds medical research aimed at developing treatments and the cure for Progeria. PRF also has its own Cell and Tissue Bank that provides the biological materials researchers need to conduct their experiments. Additionally, PRF has a Medical and Research Database – a centralized collection of medical information from Progeria patients worldwide. The data are rigorously analyzed to help us understand more about Progeria and devise treatment recommendations.
The Progeria Research Foundation funds medical research aimed at developing treatments and the cure for Progeria. PRF also has its own Cell and Tissue Bank that provides the biological materials researchers need to conduct their experiments. Additionally, PRF has a Medical and Research Database – a centralized collection of medical information from Progeria patients worldwide. The data are rigorously analyzed to help us understand more about Progeria and devise treatment recommendations.
To help answer many questions on caring for someone with Progeria, PRF published The Progeria Handbook for families and doctors. From basic health facts to daily care recommendations to extensive treatment guidelines, the handbook provides a supportive resource to help optimize quality of life for people with Progeria across the globe. The most recent edition of the Handbook is available in English, Spanish, Japanese, Portuguese, Italian, Arabic and Chinese. The handbook will also be available in other languages.
PRF is also driving Progeria clinical drug trials that are testing potential treatments, and to date, has funded and co-coordinated four clinical trials. PRF is leaving no stone unturned in our exploration of promising drugs that will bring us closer to the cure.
What can you do to help children with Progeria?
- Make a financial contribution. Donations are always needed to continue PRF’s lifesaving work. No donation is too little or too big – every dollar counts in our quest for the cure! Online donations are accepted at Give.
- Donate your time. Volunteers are also important to PRF’s success. Hold a special event like a bake sale or car wash; translate documents for the families; help with a mailing – we’ll find something for you to do that fits your schedule, location and talents! Visit our Get Involved page to see all the ways you can help.
- Learn more, spread the word, and get connected. Want to learn more about the many vital programs and services PRF offers the children and young adults with Progeria? Check out our website at progeriaresearch.org
Do you know anyone who can help? Tell your friends, family and colleagues about PRF and the lifesaving work we do! Many times, people are more likely to donate to an organization if they’ve gotten a recommendation from someone they know. So put in a good word for us and tell everyone to follow us on X@progeria, “like” us on Facebook, check out our photos on Instagram @progeriaresearch, get to know the Progeria community through some YouTube videos, and contact us directly at info@progeriaresearch.org.We look forward to connecting with you!
TOGETHER WE WILL FIND THE CURE!
[1] Other Progeroid syndromes include Werner’s syndrome, also known as “adult progeria” which does not have an onset until the late teen years, with a lifespan into the 40’s and 50’s.
[2] For a map of where living children reside, please go to https://www.progeriaresearch.org/meet-the-kids/.
[3] “Recurrent de novo point mutations in lamin A cause Hutchinson-Gilford Progeria Syndrome,” Nature, Vol. 423, May 15, 2003.
[4] 2021 American Heart Association Heart Disease and Stroke Statistics.
[5] Gordon LB, Kleinman ME, et al. Clinical trial of a farnesyltransferase inhibitor in children with Hutchinson-Gilford progeria syndrome. Proc Natl Acad Sci U S A. 2012 Oct 9;109(41):16666-71. doi: 10.1073/pnas.1202529109. Epub 2012 Sep 24.
[6] Gordon LB, Shappell H, Massaro J, et al. Association of Lonafarnib Treatment vs No Treatment With Mortality Rate in Patients With Hutchinson-Gilford Progeria Syndrome. JAMA. 2018;319(16):1687–1695.
[7] Gordon, L.B., Norris, W., Hamren, S., et al. Plasma Progerin in Patients with Hutchinson-Gilford Progeria Syndrome: Immunoassay Development and Clinical Evaluation. Circulation, 2023.
[8] Gordon LB, Basso S, et al. Intervention for critical aortic stenosis in Hutchinson-Gilford progeria syndrome. Front. Cardiovasc. Med. 11:1356010. doi: 10.3389/fcvm.2024.1356010 (2024).
[9] Koblan, L.W., Erdos, M.R., Wilson, C. et al. In vivo base editing rescues Hutchinson–Gilford progeria syndrome in mice. Nature 589, 608–614 (2021).
[10] Erdos, M.R., Cabral, W.A., Tavarez, U.L. et al. A targeted antisense therapeutic approach for Hutchinson–Gilford progeria syndrome. Nat Med (2021). https://doi.org/10.1038/s41591-021-01274-0
[11] Puttaraju, M., Jackson, M., Klein, S. et al. Systematic screening identifies therapeutic antisense oligonucleotides for Hutchinson–Gilford progeria syndrome. Nat Med (2021). https://doi.org/10.1038/s41591-021-01262-4
[12] Kang SM, Yoon MH, et al. Progerinin, an optimized progerin-lamin A binding inhibitor, ameliorates premature senescence phenotypes of Hutchinson-Gilford progeria syndrome. Commun Biol. 2021 Jan 4; 4(1):5.
[13] Gordon, L.B., Norris, W., Hamren, S., et al. Plasma Progerin in Patients with Hutchinson-Gilford Progeria Syndrome: Immunoassay Development and Clinical Evaluation. Circulation, 2023